Embark on an educational journey with the Lewis Med Surg Nursing Test Bank, your trusted companion for mastering the complexities of medical-surgical nursing. Delve into a world of in-depth knowledge, practical insights, and engaging case studies, all meticulously crafted to empower you in providing exceptional patient care.
Our comprehensive test bank covers a vast array of topics, from nursing assessment and care planning to pharmacology, fluid and electrolyte balance, wound care, infection control, critical care nursing, and more. Each section is meticulously organized and presented in a clear and concise manner, ensuring your understanding and retention of key concepts.
Nursing Assessment and Care Planning
Nursing assessment and care planning are crucial components of medical-surgical nursing. The assessment process involves gathering and analyzing data to identify patient needs and establish a comprehensive care plan.
The nursing assessment process typically includes:
- Health history
- Physical examination
- Psychosocial assessment
- Environmental assessment
Once the assessment is complete, the nurse develops a care plan that Artikels the patient’s needs, goals, and interventions. There are various types of care plans, including:
- Problem-oriented care plans
- Goal-oriented care plans
- Nursing care plans
Common nursing diagnoses for medical-surgical patients include:
- Acute pain
- Impaired mobility
- Risk for infection
Corresponding nursing interventions for these diagnoses may include:
- Administering pain medication
- Assisting with ambulation
- Implementing infection control measures
Pharmacology
Pharmacology is the study of drugs and their effects on living organisms. It encompasses the discovery, development, mechanism of action, absorption, distribution, metabolism, excretion, and adverse effects of drugs.
In medical-surgical nursing, pharmacology plays a crucial role in the safe and effective administration of medications to patients. Nurses must have a thorough understanding of pharmacology to ensure that medications are used appropriately and to minimize potential adverse effects.
Routes of Medication Administration
Medications can be administered through various routes, each with its advantages and disadvantages. The choice of route depends on factors such as the drug’s properties, the patient’s condition, and the desired onset of action.
- Oral:Convenient and cost-effective; suitable for drugs that are absorbed well from the gastrointestinal tract. Disadvantages include potential for nausea, vomiting, and delayed absorption.
- Intravenous (IV):Rapid onset of action; suitable for drugs that need to be delivered quickly or in high concentrations. Disadvantages include risk of infection, thrombosis, and extravasation.
- Intramuscular (IM):Moderate onset of action; suitable for drugs that are not well absorbed orally or need to be administered in a depot form. Disadvantages include pain and tissue irritation.
- Subcutaneous (SC):Slow onset of action; suitable for drugs that are absorbed slowly or need to be administered over a prolonged period. Disadvantages include risk of infection and tissue irritation.
- Transdermal:Slow onset of action; suitable for drugs that need to be delivered over a prolonged period or for local effects. Disadvantages include potential for skin irritation and allergic reactions.
Major Drug Classifications
Drugs are classified into different groups based on their pharmacological effects. The following table summarizes the major drug classifications, their mechanisms of action, and common side effects:
| Drug Classification | Mechanism of Action | Common Side Effects |
|---|---|---|
| Antibiotics | Kill or inhibit the growth of bacteria | Nausea, vomiting, diarrhea, rash |
| Antivirals | Inhibit the replication of viruses | Nausea, vomiting, diarrhea, headache |
| Antifungals | Kill or inhibit the growth of fungi | Nausea, vomiting, diarrhea, liver damage |
| Antiparasitics | Kill or inhibit the growth of parasites | Nausea, vomiting, diarrhea, headache |
| Analgesics | Relieve pain | Nausea, vomiting, constipation, drowsiness |
| Anti-inflammatories | Reduce inflammation | Nausea, vomiting, diarrhea, stomach ulcers |
| Cardiovascular drugs | Treat heart and blood vessel conditions | Dizziness, lightheadedness, palpitations, edema |
| Neurological drugs | Treat neurological conditions | Dizziness, drowsiness, headache, seizures |
| Endocrine drugs | Treat hormonal imbalances | Weight gain, fluid retention, mood changes |
| Chemotherapy drugs | Kill cancer cells | Nausea, vomiting, diarrhea, hair loss |
Fluid and Electrolyte Balance
Fluid and electrolyte balance is a critical aspect of maintaining homeostasis in the human body. It involves the regulation of the body’s water content, electrolyte concentrations, and acid-base balance.
Types of Fluid and Electrolyte Imbalances
Fluid and electrolyte imbalances can be classified into two main types:
- Hypervolemia: Excess fluid volume in the body
- Hypovolemia: Decreased fluid volume in the body
Electrolyte imbalances can involve either an excess or deficiency of specific electrolytes, such as sodium, potassium, calcium, or magnesium.
Clinical Manifestations of Fluid and Electrolyte Imbalances
The clinical manifestations of fluid and electrolyte imbalances vary depending on the type and severity of the imbalance. Some common signs and symptoms include:
- Hypervolemia: Edema, hypertension, shortness of breath
- Hypovolemia: Dehydration, hypotension, tachycardia
- Hypernatremia: Confusion, seizures, coma
- Hyponatremia: Headache, nausea, seizures
- Hyperkalemia: Muscle weakness, cardiac arrhythmias
- Hypokalemia: Muscle weakness, fatigue, nausea
- Hypercalcemia: Bone pain, nausea, confusion
- Hypocalcemia: Muscle cramps, tetany, seizures
Interventions for Fluid and Electrolyte Imbalances
The interventions for fluid and electrolyte imbalances depend on the specific type and severity of the imbalance. Common interventions include:
| Imbalance | Intervention |
|---|---|
| Hypervolemia | Diuretics, fluid restriction |
| Hypovolemia | Intravenous fluids, electrolytes |
| Hypernatremia | Intravenous fluids (D5W) |
| Hyponatremia | Intravenous fluids (3% NaCl) |
| Hyperkalemia | Intravenous calcium, potassium-lowering medications |
| Hypokalemia | Intravenous potassium, potassium supplements |
| Hypercalcemia | Intravenous fluids, bisphosphonates |
| Hypocalcemia | Intravenous calcium, vitamin D supplements |
Wound Care
Wound care is the management of wounds to promote healing and prevent infection. The principles of wound care include:
- Cleaning the wound to remove debris and bacteria.
- Controlling bleeding.
- Protecting the wound from further injury.
- Promoting healing by providing a moist environment and removing dead tissue.
- Preventing infection by using antibiotics and other medications.
Types of Wounds
There are many different types of wounds, each with its own unique management. Some of the most common types of wounds include:
- Abrasions: These are superficial wounds that involve the top layer of skin.
- Lacerations: These are cuts that are caused by a sharp object.
- Puncture wounds: These are wounds that are caused by a sharp object that pierces the skin.
- Contusions: These are bruises that are caused by a blunt object.
- Burns: These are wounds that are caused by heat, chemicals, or electricity.
Wound Dressings
Wound dressings are used to protect wounds from further injury and infection, and to promote healing. There are many different types of wound dressings available, each with its own unique properties. Some of the most common types of wound dressings include:
| Type of Dressing | Indications |
|---|---|
| Gauze | Superficial wounds with minimal drainage |
| Hydrocolloid dressings | Moderate to heavily draining wounds |
| Foam dressings | Wounds with deep pockets or tunneling |
| Alginate dressings | Wounds with heavy drainage or exudate |
| Transparent film dressings | Superficial wounds that need to be monitored |
Infection Control
Infection control refers to the practices and procedures used to prevent the spread of infections in healthcare settings. It involves identifying, preventing, and controlling the transmission of infectious agents to protect patients, healthcare workers, and the community.
Principles of Infection Control
The principles of infection control include:
- Standard precautions: These are applied to all patients regardless of their suspected or confirmed infection status.
- Transmission-based precautions: These are additional precautions taken when caring for patients with known or suspected infections that can be transmitted through specific routes, such as airborne, droplet, or contact.
- Environmental cleaning and disinfection: Regular cleaning and disinfection of surfaces, equipment, and patient care areas is essential to prevent the spread of infections.
- Hand hygiene: Proper hand hygiene is the most important measure to prevent the spread of infections.
- Personal protective equipment (PPE): PPE, such as gloves, gowns, and masks, is used to protect healthcare workers from exposure to infectious agents.
Types of Infections and Transmission
Infections can be classified based on the type of infectious agent and the route of transmission. Common types of infections include:
- Bacterial infections: Caused by bacteria, such as Staphylococcus aureusor Escherichia coli, and can be transmitted through contact with contaminated surfaces or objects, or through respiratory droplets.
- Viral infections: Caused by viruses, such as influenza or COVID-19, and can be transmitted through respiratory droplets, contact with contaminated surfaces, or through blood or bodily fluids.
- Fungal infections: Caused by fungi, such as Candidaor Aspergillus, and can be transmitted through contact with contaminated surfaces or objects, or through inhalation of fungal spores.
- Parasitic infections: Caused by parasites, such as Plasmodium(malaria) or Toxoplasma gondii(toxoplasmosis), and can be transmitted through contact with contaminated food or water, or through insect bites.
Common Interventions for Preventing and Treating Infections
| Intervention | Purpose |
|---|---|
| Standard precautions | Prevent the spread of infections regardless of the suspected or confirmed infection status. |
| Transmission-based precautions | Prevent the spread of specific infections that can be transmitted through specific routes. |
| Environmental cleaning and disinfection | Remove and kill infectious agents from surfaces, equipment, and patient care areas. |
| Hand hygiene | Prevent the transmission of infections through contact with contaminated hands. |
| Personal protective equipment (PPE) | Protect healthcare workers from exposure to infectious agents. |
| Immunizations | Prevent or reduce the severity of infections by providing immunity. |
| Antimicrobial therapy | Treat infections caused by bacteria, viruses, or fungi. |
Critical Care Nursing: Lewis Med Surg Nursing Test Bank
Critical care nursing is a specialized area of nursing that focuses on the care of critically ill patients. These patients require close monitoring and intensive interventions to maintain their vital functions and prevent further deterioration. Critical care nurses are highly skilled and experienced in managing complex medical conditions and providing life-saving interventions.
Principles of Critical Care Nursing
The principles of critical care nursing include:
- Maintaining vital functions: Critical care nurses monitor and maintain vital functions such as blood pressure, heart rate, respiratory rate, and oxygen saturation.
- Early detection and intervention: Critical care nurses are trained to detect subtle changes in a patient’s condition and intervene promptly to prevent complications.
- Collaborative care: Critical care nurses work closely with physicians, respiratory therapists, and other healthcare professionals to provide comprehensive care to patients.
- Patient and family support: Critical care nurses provide support and education to patients and their families during a stressful time.
Types of Critical Care Patients
Critical care patients come from a variety of backgrounds and have a wide range of medical conditions. Some common types of critical care patients include:
- Cardiac patients: Patients with heart attacks, arrhythmias, or other cardiac conditions.
- Respiratory patients: Patients with pneumonia, acute respiratory distress syndrome (ARDS), or other respiratory conditions.
- Neurological patients: Patients with stroke, traumatic brain injury, or other neurological conditions.
- Trauma patients: Patients who have suffered major trauma, such as a car accident or a gunshot wound.
- Medical patients: Patients with sepsis, organ failure, or other medical conditions.
Management of Critical Care Patients
The management of critical care patients involves a variety of interventions, including:
- Mechanical ventilation: Mechanical ventilation is used to support breathing in patients who are unable to breathe on their own.
- Vasopressors: Vasopressors are medications that are used to increase blood pressure in patients who are hypotensive.
- Inotropes: Inotropes are medications that are used to increase the strength of the heart’s contractions.
- Antiarrhythmics: Antiarrhythmics are medications that are used to treat arrhythmias.
- Sedatives and analgesics: Sedatives and analgesics are used to keep patients comfortable and reduce pain.
| Intervention | Purpose |
|---|---|
| Mechanical ventilation | To support breathing |
| Vasopressors | To increase blood pressure |
| Inotropes | To increase the strength of the heart’s contractions |
| Antiarrhythmics | To treat arrhythmias |
| Sedatives and analgesics | To keep patients comfortable and reduce pain |
Case Studies
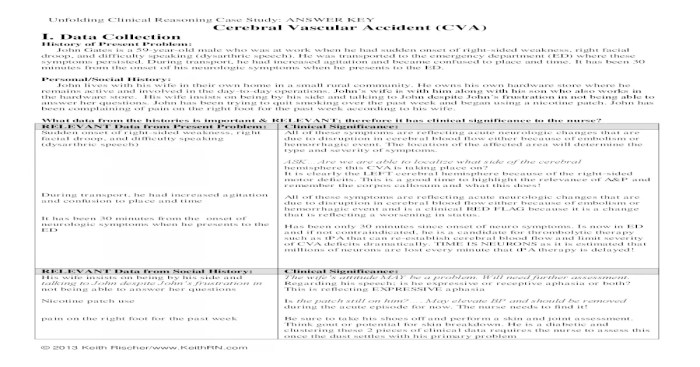
Case studies are an essential tool for medical-surgical nurses, as they provide a way to apply nursing principles to real-world situations. By studying case studies, nurses can develop their critical thinking skills, problem-solving abilities, and clinical judgment.
Each case study should include the following information:
- A brief description of the patient’s condition
- The nursing assessment
- The nursing care plan
- The evaluation of the nursing interventions
Nursing Assessment, Lewis med surg nursing test bank
The nursing assessment is the first step in the nursing process. It involves collecting data about the patient’s condition, including their medical history, physical examination, and laboratory results. The nursing assessment helps the nurse to identify the patient’s needs and develop a plan of care.
General Inquiries
What is the Lewis Med Surg Nursing Test Bank?
It is a comprehensive resource designed to help nursing students prepare for exams and master the concepts of medical-surgical nursing.
What topics are covered in the test bank?
It covers a wide range of topics, including nursing assessment and care planning, pharmacology, fluid and electrolyte balance, wound care, infection control, and critical care nursing.
How can I access the test bank?
The test bank is available for purchase through various online platforms.
Is the test bank helpful for exam preparation?
Yes, the test bank provides practice questions, case studies, and detailed explanations to enhance exam readiness.