Nursing diagnosis for herpes zoster is a critical aspect of patient care, providing a framework for understanding the patient’s condition and guiding appropriate interventions. This diagnosis encompasses the identification of defining characteristics, related factors, and risk factors associated with herpes zoster, a painful and debilitating condition caused by the varicella-zoster virus.
Herpes zoster, also known as shingles, is characterized by a painful rash that typically affects one side of the body. The virus that causes herpes zoster remains dormant in the body after a chickenpox infection and can reactivate later in life, leading to the development of shingles.
Nursing Diagnosis for Herpes Zoster
Definition of Herpes Zoster
Herpes zoster, also known as shingles, is a viral infection that causes a painful rash. It is caused by the varicella-zoster virus (VZV), the same virus that causes chickenpox. After a person has chickenpox, the virus remains dormant in the body’s nerve cells.
Years later, the virus can reactivate and cause herpes zoster.
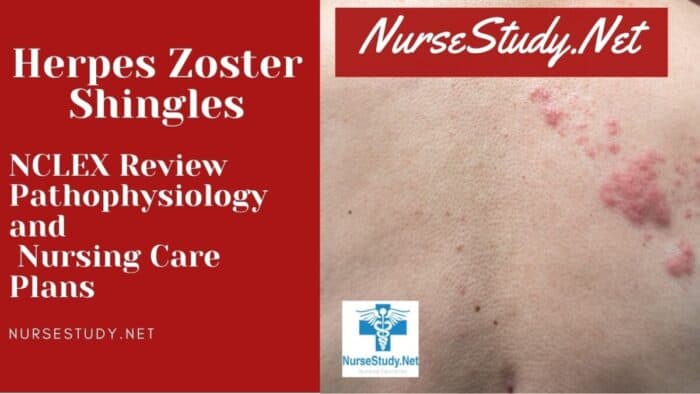
Signs and Symptoms of Herpes Zoster
The most common symptom of herpes zoster is a painful rash. The rash typically appears on one side of the body and can be accompanied by blisters, itching, and burning. Other symptoms of herpes zoster can include:
- Fever
- Chills
- Fatigue
- Headache
- Muscle aches
- Nausea
- Vomiting
Pathophysiology of Herpes Zoster
The pathophysiology of herpes zoster is not fully understood. However, it is believed that the virus reactivates when the body’s immune system is weakened. This can occur due to a variety of factors, including stress, illness, or certain medications. Once the virus is reactivated, it travels along the nerve fibers to the skin, where it causes the characteristic rash.
Risk Factors for Herpes Zoster
Herpes zoster, commonly known as shingles, is a viral infection that causes a painful rash. The virus that causes herpes zoster is the varicella-zoster virus (VZV), which is the same virus that causes chickenpox. After a person has chickenpox, the virus remains dormant in the body’s nerve cells.
Years later, the virus can reactivate and cause herpes zoster.
Several risk factors increase the likelihood of developing herpes zoster. These risk factors include:
Age
The risk of developing herpes zoster increases with age. People over the age of 50 are at the highest risk.
Immune Status
People with weakened immune systems are more likely to develop herpes zoster. This includes people with HIV/AIDS, cancer, or those taking immunosuppressant medications.
Stress, Nursing diagnosis for herpes zoster
Stress can trigger the reactivation of the varicella-zoster virus. This is because stress can weaken the immune system.
Underlying Medical Conditions
Certain underlying medical conditions can also increase the risk of developing herpes zoster. These conditions include diabetes, chronic lung disease, and kidney disease.
Complications of Herpes Zoster
Herpes zoster, commonly known as shingles, can lead to various complications if not diagnosed and treated promptly. These complications can range from mild to severe and can significantly impact an individual’s quality of life.
The most common complication of herpes zoster is postherpetic neuralgia (PHN), which affects approximately 10-20% of individuals who develop shingles. PHN is characterized by persistent pain that lasts for more than three months after the shingles rash has healed. The pain can be severe and debilitating, affecting an individual’s ability to perform daily activities and sleep.
Ocular Complications
Herpes zoster can also affect the eyes, leading to a condition known as herpes zoster ophthalmicus. This occurs when the virus affects the nerves that supply the eye, causing inflammation and pain. Herpes zoster ophthalmicus can lead to serious complications such as corneal scarring, uveitis, and even vision loss.
Neurological Complications
In rare cases, herpes zoster can spread to the central nervous system, causing neurological complications such as encephalitis, meningitis, and Guillain-Barré syndrome. These complications can be life-threatening and require immediate medical attention.
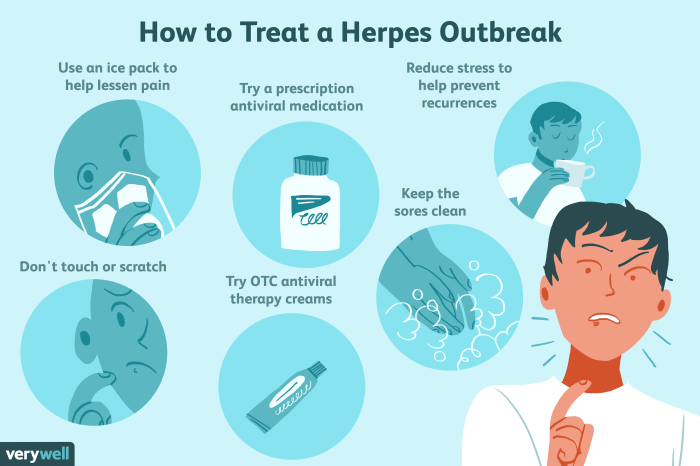
Early diagnosis and treatment of herpes zoster are crucial to prevent the development of complications. Antiviral medications can be used to reduce the severity and duration of the rash and the risk of PHN. In addition, pain relievers and other medications can be used to manage the symptoms of PHN.
Nursing Management of Herpes Zoster: Nursing Diagnosis For Herpes Zoster
Nursing management of herpes zoster aims to alleviate symptoms, prevent complications, and provide patient education and support. The nursing care plan encompasses pain management, antiviral therapy, supportive care, and patient education.
Pain Management
Pain is a common symptom of herpes zoster. Nurses play a crucial role in assessing and managing pain effectively. They may administer analgesics, such as nonsteroidal anti-inflammatory drugs (NSAIDs) or opioids, as prescribed by the healthcare provider. Topical pain relievers, such as capsaicin cream, can also provide localized pain relief.
Antiviral Therapy
Antiviral medications, such as acyclovir, valacyclovir, and famciclovir, are prescribed to inhibit the replication of the varicella-zoster virus. Early initiation of antiviral therapy can reduce the severity and duration of symptoms. Nurses monitor patients for adverse effects of antiviral medications, such as nausea, vomiting, and diarrhea.
Supportive Care
Supportive care measures aim to promote patient comfort and prevent complications. Nurses provide skin care to prevent infection and promote healing of the rash. They also encourage rest and adequate hydration. Nutritional support is essential to maintain the patient’s strength and overall well-being.
Patient Education and Support
Patient education is crucial in herpes zoster management. Nurses educate patients about the disease, its symptoms, and treatment options. They also provide information on preventing the spread of infection to others. Emotional support is equally important, as herpes zoster can cause significant distress and anxiety.
Nurses provide a listening ear, offer reassurance, and connect patients with support groups or other resources.
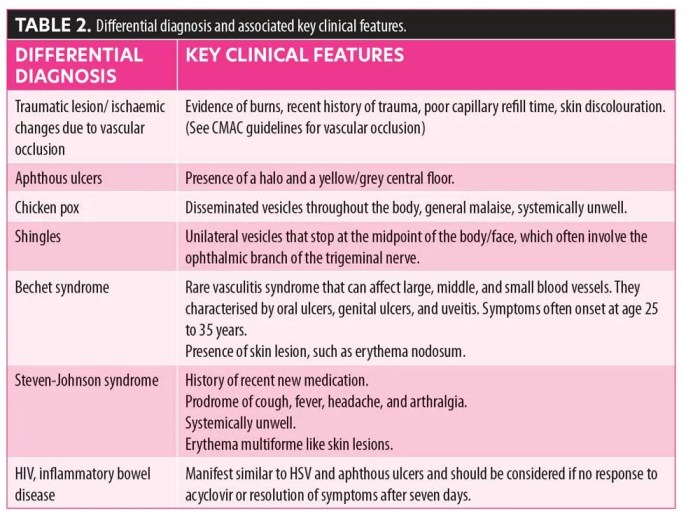
Differential Diagnosis of Herpes Zoster
Herpes zoster, also known as shingles, is a viral infection that causes a painful rash. It is important to differentiate herpes zoster from other conditions with similar symptoms, such as herpes simplex virus (HSV), varicella-zoster virus (VZV), and other skin conditions.
A thorough medical history and physical examination are crucial for an accurate diagnosis. The healthcare provider will inquire about the patient’s symptoms, including the duration, location, and characteristics of the rash. They will also assess the patient’s overall health and any underlying conditions that may contribute to the symptoms.
Diagnostic Tests
In some cases, diagnostic tests may be necessary to confirm the diagnosis of herpes zoster. These tests may include:
- Viral culture:A sample of the fluid from the blisters is collected and tested in a laboratory to identify the virus.
- Polymerase chain reaction (PCR) test:This test detects the genetic material of the virus in a sample of the fluid from the blisters.
- Serology test:This test measures the antibodies in the blood that are produced in response to the virus.
These tests can help to distinguish herpes zoster from other conditions with similar symptoms and ensure that the patient receives appropriate treatment.
Health Promotion and Prevention of Herpes Zoster
Herpes zoster, commonly known as shingles, is a viral infection that causes a painful rash. While there is no cure for herpes zoster, it can be prevented and managed effectively. Health promotion and prevention strategies play a crucial role in reducing the incidence and severity of herpes zoster.
Vaccination
Vaccination is the most effective way to prevent herpes zoster. The herpes zoster vaccine is recommended for adults over 50 years of age. The vaccine is safe and effective in reducing the risk of developing herpes zoster by up to 50%. It is also effective in reducing the severity of the rash and the risk of complications.
Lifestyle Modifications
Certain lifestyle modifications can help reduce the risk of developing herpes zoster. These include:
- Maintaining a healthy weight
- Eating a healthy diet
- Getting regular exercise
- Reducing stress
- Getting enough sleep
Recommendations
To promote health and prevent herpes zoster, it is recommended that adults over 50 years of age get vaccinated. Additionally, everyone should follow a healthy lifestyle that includes a balanced diet, regular exercise, and adequate sleep. By following these recommendations, individuals can significantly reduce their risk of developing herpes zoster.
Questions and Answers
What are the common signs and symptoms of herpes zoster?
Herpes zoster typically presents with a painful rash that appears on one side of the body, often in a band-like distribution. The rash is accompanied by blisters, itching, and burning sensations.
What are the risk factors for developing herpes zoster?
Age, weakened immune system, and certain medical conditions, such as cancer and HIV/AIDS, increase the risk of developing herpes zoster.
What are the potential complications of herpes zoster?
Herpes zoster can lead to serious complications, including postherpetic neuralgia, ocular complications, and neurological complications.
What is the treatment for herpes zoster?
Treatment for herpes zoster involves pain management, antiviral therapy, and supportive care. Early diagnosis and treatment are essential to prevent complications.